Sunday, April 7, 2019
Minefield Called Ayushman Bharat — Thoughts on Way Forward
The nobility in thought of this Government to bring a comprehensive healthcare intervention is appreciable. In his budget announcement, Shri Arun Jaitely said that the Ayushman Bharat program will help build a New India 2022 to ensure enhanced productivity, wellbeing and avert wage loss and impoverishment. It has a planned timeline of 4 years for realising the impact of intervention. This program will have two parts, Health and Wellness Center (HWC) a foundation level care and a State sponsored insurance scheme for secondary and tertiary care called National Health Protection Scheme (NHPS). However it isn’t certain if the general elections of 2019 and its refractory period to effect major changes in Governmental process has been factored in the calculation.
Any major reform that an elected Government hopes to succeed is usually brought about in the beginning of its term. This allows them to constantly course correct and most importantly help establish systems. Programs/ announcements focusing on employability such as Make in India, Skill India, Startup India all came in the early days of the present Government. Significant financial interventions like demonetisation and GST were introduced in the first half of the Governments term too. It is interesting to note that a significant healthcare intervention requiring substantial systemic stabilisation has been brought about in the death hours of its term.
Whilst there are multiple propositions on the relative success of each of the previous interventions, there is none that definitely puts it in either basket. Going to the electorate with even partial indication of failure on a program that has plenty of mind space captured by pervasive publicity, is a risky proposition. It is interesting to note that the Government and its advisors are willing to take its chances of introducing a major welfare measure during the death hours of its current term.
Multiple statements from the Governments Think-tank Niti Ayog, MoHFW and Finance ministry indicate that the planning for the program is still underway and the announcement have preceded it. A policy without planning of its implementation details is a great vision statement that works as a picturesque frame on the wall. However when it is made for a welfare measure for the public who have been primed heavy to expect ache din and not implemented for want of detailed planning, is bound to be a Bhure din for the political establishment or at least one more irritant that pushes them into the valley of death.
There is limited leverage that the Union Government has over the States on healthcare delivery. This is primarily because the money spent on healthcare comes predominantly from the States’ budget. Furthermore, States are the principal agents in the delivery of healthcare. Health is a basal need issue and acts as an important political touch point with public. Therefore elected Governments, irrespective of their ideological predisposition, will try their best to have a direct control on the healthcare service delivery. With growing awareness, public have started to express their demands for higher service quality. It is therefore quintessential for the Union and State Governments to work together leveraging existing channels and improving service quality.
Multiplicity of offices and establishments trying to address the implementation of Ayushman Bharat can create a significant amount of media reports and thereby enhanced expectation among the public. However in reality this spotlighting of a program is likely to be deleterious for an impactful implementation. It is pertinent that an effective interim nodal office is established to help build the system and laterally implement good practices. MoHFW being the line ministry for health and family welfare, the office could be within this Ministry with reasonable teeth and outside the regular reporting chains of bureaucracy. The regular bureaucracy will be an excellent establishment to run established system. However, it is neither primed nor equipped to experiment or bring about disruptive innovations.
A workable long term solution for the execution of major programs like Ayushman Bharat, particularly the NHPS, will be to have an independent regulatory authority created by an act of parliament, say National Health Authority (NHA). It will be important to keep this independent authority away from reporting to the bureaucracy of the line ministry, particularly for its financial existence. NHA act should be transparent in operations and continually made stronger by bringing amendments to respond to ground realities.
Care should be taken in populating the leadership of NHA, at least in the early phases. It is important to have disruptive thinking leaders who could learn from ground reality in an unstructured way and have an eye for brining in standardisation and structured execution. A visionary executive can pave the way and help create systems that can be standardised to run within the bureaucratic system in future. It has been observed that disruptive changes can be brought better to the table by people who are not part of the existing bureaucratic structure thereby avoiding egos of batch and rank seniority during interaction.
Furthermore, best practices from across the Union on programs that are running successfully such as TN and KL should be implemented in NHPS. This would be a better and easily implementable model over the hugely expensive NHS of Britain.
Of the two parts of Ayushman Bharat, the Health and Wellness Centres (HWC) is relatively easy to be established. This is primarily due to the fact that it is a work already being performed under different schemes of National Health Mission (NHM), of MoHFW. The Cost for establishing the centres are easy to estimate and might have been apportioned in the Union Budget.
Ayushman Bharat presents a key opportunity to help establish good systems and tracking of the HWC program. There probably is no system or product that has been created perfect. Perfection emerges from cumulative improvement by a prepared mind that sense opportunities with ease. It is that prepared mind (system) that has to be established while implementing the program. Best practices from various domains that have evolved mechanisms to identify opportunities for improvement and implement them should be leveraged in establishing HWC.
While the NHPS looks attractive from the problem size, it is important to focus on the HWC of Ayushman Bharat. Most major complications can be addressed by working on the wellness at the primary care. For instance, a patient presenting with hypertension with managed diet and exercises is less likely to graduate for availing the facilities of NHPS in the form of cardiac or other ailments. Therefore a sharp focus on HWC will have a significant impact in reducing the burden of disease under NHPS.
Reducing wastes at the delivery point can reduce the cost of treatment and can be easily built across the spectrum from wellness center to tertiary care provider. NHA can help build processes and guidelines to effectively implement it by giving adequate training. Owing to the large scale and distributed nature of working, it is important to have an IT backbone to help the system stand up. However, it is a well understood fact that any system that doesn’t have a well-defined process will not provide a good performance, merely by the availability of better IT systems. While IT is a great enabler, it comes just after systems are put in place. Office of NHA can help moderate this infrastructure development by taking into cognisance the other IT developments that have happened over time.
Health is as much about human resource (HR) availability as it is for technology and infrastructure. The doctor-to-population ratio for India is at about 1,655 per doctor with a skewness of about 3.8 doctors in the urban area for one in rural. It is estimated that there is a 24.4% doctor shortage in PHC and 81.8% specialists at community health centres. Hence systems to incentivise or making it mandatory for migration of doctors is required in the short term. This necessitates major intervention from the political leadership from across the spectrum. Starting of new medical colleges may not be the only solution as it takes about 5.5 years to get trained MBBS doctors and specialists between 4-6 years after that.
To further add to this urban-rural skewness is the geographic distribution across regions. The southern states have a higher penetration and availability of both physical infrastructure and HR. In the short term, it will be difficult to move HR into less penetrated Northern region. Therefore the insurance payoffs will tend to go to already performing (southern) States. Thereby this will create a positive feedback to the system, i.e., the needy will tend to go to Southern States, who will get more insurance payoffs and will further develop infrastructure to attract more patients. The states that have lesser capacity as off today will tend to have an operational issue of subsidising the development of more capacity states. This will be a political dilemma and most states that are not politically aligned to the center may have reservations to pursue NHPS program of Ayushman Bharat.
To address the geographic skewness and have an effective responsive system, it will be important to move away from the Delhi centric model to a cluster/ regional model. Whilst the NHA Headquarters could be based out of Delhi and managing the city/ state of Delhi. It is important to create five (5) regional offices for overseeing the work in their respective regions in addition to the offices to liaison directly with the governments in each state and union territory. In the initial years, pooled results will have southern region compensating for the north and giving them a positive target to focus. If concerted efforts are made, it would be feasible to establish parity in service delivery across the country in about a decade. Some of the suggested locations for the regional offices could be as follows:
Southern with HQ in Chennai (TN, KL, KA, AP, TL, PY, AN)
Western with HQ in Mumbai (MH, GJ, RJ, GA, DD, DN, LD)
Eastern with HQ in Lucknow (UP, MP, CG, JH, BR, WB)
Northern with HQ in Chandigarh (CH, HR, PB, HP, JK, UK)
North-eastern with HQ in Guwahati (AS, TR, ML, NL, MN, MZ, AR)
It would be ideal to retain Government insurance companies in the early stages of NHPS. This is primarily due to the difficulty of having a clear forecast of outflow for the insurance without any prior data. Furthermore, insurance companies will have lesser operational issues in reconciling and adjustment across regions arising from the differences in payout. For instance, there is an expectation in the short term owing to HR and capacity shortages, patients will tend to go from a Northern or Eastern state to a Southern State. Hence there will be a need to move the insurance outflow between companies that can happen best if the insurance provider is State owned.
One of the advantages with such a large insurance program is the scale of procurement. If there is a diligent, transparent and simple system established; the cost of procurement and care delivery can be greatly reduced. This can have a secondary effect in bringing down the overall cost of healthcare delivery. Successful reduction in cost can happen only if we deploy a strong interdisciplinary teams of doctors, academics, engineers and finance trained people. This essentially implies that if NPPA is brought under the NHA office, there will be cohesive procurement and contracts that can be ensured. NHA will also have tooth to break cartels and help provide transparent health technology assessment to the public.
It will be the constraints called detailed planning and systems that would limit Ayushman Bharat to have a perceivable and palpable outcomes. It is important to focus the Government’s efforts on building systems for implementation and not limit it to media blitzkrieg to capture mind space. The nation across its length and breadth feels the impact of interventions on the ground that their mind space is peppered to expect. Policy makers, at least the elected, might want to consider this to avoid repeating “Shining India” of 2004 in 2019.
The biggest leverage that can be obtained from this healthcare intervention is the incentive for indigenously developed products, particularly from Start-ups, to be used extensively. There is an excellent opportunity for innovators to work on solutions that can bring the cost of care delivery down. Some structural changes to the system such as, simpler licensing policy; reduction of entry barrier created by an invisible cartel of device manufacturers, practitioners and hospitals, and other changes can be implemented. This will lead to concomitant improvement and success of 3 major interventions of the current Government for the New India, i.e., Start-up India, MakeInIndia and Ayushman Bharat.

Minefield Called Ayushman Bharat — Thoughts on Way Forward
Related Articles
-

A Made-in-India patch to mend hearts
-
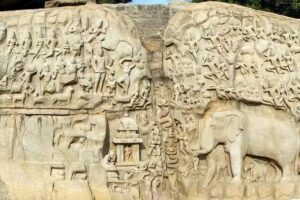
Mamallapuram: Then And Now
-

IIT Madras generated ₹1,081 crore from govt projects and industry consultancy in 2021-22
-

Tamil Nadu receives Best Performance in Road Safety award
-

Outcome of Data-Driven Policy Initiatives in Tamil Nadu
-

Disaster, another disaster, and then disaster Management
